-
Featured News
Mayo Clinic Q and A: Painful bowel movements may be due to anal fissure
 DEAR MAYO CLINIC: I’ve been having painful bowel movements for about a month. I thought they were caused by hemorrhoids, which I’ve had on and off for years. But over-the-counter hemorrhoid medication isn’t helping at all. Could something else be causing the pain? Should I see my health care provider?
DEAR MAYO CLINIC: I’ve been having painful bowel movements for about a month. I thought they were caused by hemorrhoids, which I’ve had on and off for years. But over-the-counter hemorrhoid medication isn’t helping at all. Could something else be causing the pain? Should I see my health care provider?
ANSWER: It’s unlikely that hemorrhoids are the source of your pain. Instead, the painful bowel movements you’re experiencing are much more likely to be due to a condition called an anal fissure. Your health care provider can confirm that with an exam. Anal fissures usually don’t go away on their own, so it’s important to have the condition properly identified and treated.
It’s common for people to assume that their hemorrhoids are the cause of painful bowel movements. But, although hemorrhoids often cause itching, irritation, sensitivity and other discomfort around the affected area, hemorrhoids rarely lead to pain during a bowel movement.
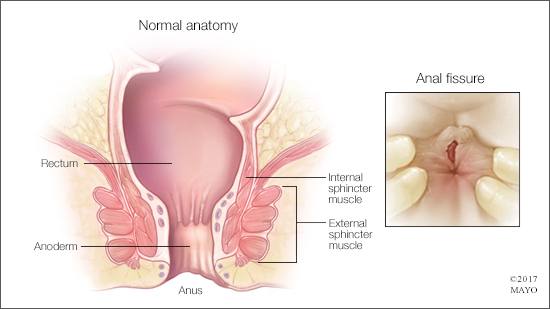
Anal fissures, however, are a frequent source of pain with bowel movements. These small tears occur in the skin around the anus or in the thin tissue that lines the anus, called the anoderm. An anal fissure may develop when you pass hard or large stools during a bowel movement. Anal fissures typically cause pain and bleeding with bowel movements.
When an anal fissure occurs, the tear can expose the ring of muscle that holds your anus closed. This ring of muscle, called the internal sphincter muscle, lies underneath the anal skin and tissue. That exposure may trigger spasms in the sphincter muscle. The spasms often trigger more pain, and they also prevent the fissure from healing. This sets up a vicious cycle of continuing pain.
A physical exam is typically all that’s needed to diagnose an anal fissure accurately. Treatment is completed in stages. How much treatment you need depends on how severe the fissure is and how well it responds to the initial treatment.
The first step in treatment is to increase the amount of fluid and fiber in your diet to make stools softer and easier to pass. That eases pressure on the fissure during bowel movements. Taking a bulking agent, such as Metamucil, Benefiber or Citrucel, can help.
If the fissure doesn’t heal within several weeks, the next step is to use a topical medication that’s applied to the skin to increase blood flow to the fissure, promote healing and help the sphincter muscle relax, thereby decreasing spasms. A topical form of nitroglycerin or the calcium channel blocker nifedipine is often used for this purpose.
If the fissure persists despite these therapies, your health care provider may recommend an injection of botulinum toxin type A (Botox) into the internal sphincter muscle. That eases spasms by paralyzing the muscle.
Finally, if a fissure still doesn’t heal with the other treatments, you may need surgery. A procedure called lateral internal sphincterotomy typically is used to treat chronic anal fissures. It involves cutting a small area of the internal sphincter muscle to reduce spasms and pain. Research has shown that, for a fissure that doesn’t heal over time with medical treatment, surgery is often effective. The procedure does, however, carry a small risk of causing brief incontinence to gas.
Make an appointment to see your health care provider, and have your situation evaluated. If it is an anal fissure causing pain during bowel movements, it’s important to start treatment as soon as possible to promote healing and prevent further damage. — Dr. John Pemberton, Colon and Rectal Surgery, Mayo Clinic, Rochester, Minnesota
Related Articles